Issue Archive
Table of Contents
BLOOD COMMENTARIES
REVIEW ARTICLE
PI3Kγ in leukemia: class IB PI3 kinase reemerges as a cancer-intrinsic target
Phosphoinositide 3-kinase gamma (PI3Kγ), long recognized as a cell-extrinsic immunotherapy target in solid tumors, is now emerging as a cell-intrinsic dependency in acute myeloid leukemia (AML) under specific conditions. Luo et al review recent studies that support PI3Kγ inhibition as a promising monotherapy or combination strategy in AML, prompting clinical trials and parallel research to identify biomarkers of response. Key questions remain regarding mechanisms of resistance, optimal combination partners, and the role of the leukemia microenvironment in modulating therapeutic efficacy.
HOW I TREAT
How I treat type 1 plasminogen deficiency
Type 1 plasminogen deficiency (PLGD) is an ultrarare genetic disorder caused by pathogenic variants in the PLG gene, leading to significantly reduced levels of both immunoreactive and functional plasminogen. This deficiency impairs the breakdown of fibrin, resulting in the accumulation of fibrin-rich pseudomembranes on mucosal surfaces, which can interfere with normal tissue and organ function. Shapiro and Nakar review the underlying biology and clinical manifestations of PLGD and present illustrative clinical vignettes to highlight key diagnostic and therapeutic considerations. The authors also discuss intravenous human plasma–derived Glu-plasminogen, the only US Food and Drug Administration–approved treatment for PLGD, which replenishes plasminogen levels and aids in the resolution of pseudomembranes.
CLINICAL TRIALS AND OBSERVATIONS
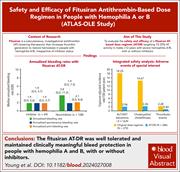
Safety and efficacy of a fitusiran antithrombin-based dose regimen in people with hemophilia A or B: the ATLAS-OLE study
Clinical Trials & Observations
Fitusiran, a subcutaneous investigational small interfering RNA antithrombin (AT)–lowering therapeutic, increases thrombin generation to restore hemostasis in people with hemophilia A or B, irrespective of inhibitor status. Thrombotic complications were seen in previous trials. Young et al report on a phase 3 open-label extension study and show that when using a different AT-based dose regimen, fitusiran was well tolerated and maintained clinically meaningful protection against bleeding in people with hemophilia A and B, with as few as 6 injections per year; thrombotic event rates were similar to those seen in the general hemophilia population. Longer follow-up is ongoing to confirm the durability of this favorable safety profile.
HEMATOPOIESIS AND STEM CELLS
cMPL-based purification and depletion of human hematopoietic stem cells: implications for pretransplant conditioning
With the increasing application of gene-corrected hematopoietic stem and progenitor cells (HSPCs) to treat nonmalignant diseases, there is a need for precise conditioning strategies that effectively deplete endogenous HSPCs to allow engraftment. Araki et al demonstrate that the thrombopoietin receptor cMPL is expressed in human long-term repopulating hematopoietic stem cells (LT-HSCs) but has minimal expression on more mature progenitors and is not expressed in nonhematopoietic tissues. The authors developed a novel conditioning approach using an anti-cMPL immunotoxin to selectively target endogenous LT-HSCs. This study provides a strong rationale for further evaluation of anti-cMPL immunotoxins as nongenotoxic conditioning regimens.
IMMUNOBIOLOGY AND IMMUNOTHERAPY
Beyond genotype: challenges in predicting disease risk for carriers of biallelic perforin variants
Clinical Trials & Observations
LYMPHOID NEOPLASIA
The bone marrow NK-cell profile predicts MRD negativity in patients with multiple myeloma treated with daratumumab-based therapy
Clinical Trials & Observations
Brief Report
Natural killer (NK) cells are important effector cells in antibody-based immune therapies for multiple myeloma through antibody-dependent cellular cytotoxicity. Korst and colleagues leveraged large patient cohorts and single-cell technologies to show that altered NK-cell distribution was associated with reduced likelihood of patients newly diagnosed with myeloma achieving measurable residual disease (MRD) negativity upon treatment with daratumumab-based regimens. These findings highlight the impact of the bone marrow NK-cell compartment on therapeutic outcomes in patients with myeloma receiving immunotherapy with CD38-targeting antibodies.
MYELOID NEOPLASIA
Blood-based proteomic profiling identifies OSMR as a novel biomarker of AML outcomes
Inflammation is increasingly recognized as playing a key role in acute myeloid leukemia (AML) pathogenesis. Through proteomic profiling on blood samples from 543 patients, Reville et al generated an 8-protein prognostic model. This Leukemia Inflammatory Risk Score outperforms the 2022 European LeukemiaNet risk model for predicting overall survival across multiple cohorts. One of these proteins, soluble oncostatin M receptor (OSMR), is strongly predictive of outcomes as a single biomarker. If further validated, these discoveries could refine risk stratification in patients with newly diagnosed AML.
THROMBOSIS AND HEMOSTASIS
Destabilization of PF4-antigenic complexes in heparin-induced thrombocytopenia
Heparin-induced thrombocytopenia (HIT) is initiated by antibodies that recognize large antigenic complexes formed by multiple cationic platelet factor 4 (PF4) molecules and polyanions such as unfractionated heparin. Rauova et al demonstrate in a murine model of HIT that universal heparin reversal agents (UHRAs) inhibit the formation of ultralarge immune complexes, dissociate preformed complexes, and suppress thrombosis. These findings support further investigation of UHRAs as a potential new therapeutic approach for HIT.
TRANSPLANTATION
Social determinants of health and access to allogeneic hematopoietic cell transplantation for acute myeloid leukemia
CME
Clinical Trials & Observations
Allogeneic hematopoietic cell transplantation (allo-HCT) remains the standard of care for many patients with acute myeloid leukemia (AML). In this month’s CME article, Wuliji et al examined whether access to allo-HCT is equitable across different social determinants of health and found that patients from lower-resourced areas are less likely to undergo allo-HCT and have higher overall mortality. Notably, even among those who do receive allo-HCT, individuals from socioeconomically disadvantaged regions experience worse outcomes. These findings underscore the need for targeted interventions to ensure equitable access to allo-HCT and improve outcomes for underserved AML patient populations.
LETTERS TO BLOOD
BLOOD WORK
CONTINUING MEDICAL EDUCATION (CME) QUESTIONS
-
Cover Image
Cover Image
![issue cover]()
Oncostatin M receptor (OSMR; green), a novel blood-based biomarker for acute myeloid leukemia (AML), is selectively expressed in CXCL12+ mesenchymal stromal cells (red), with yellow indicating colocalization of OSMR and CXCL12, in the bone marrow of a patient with AML. In contrast, CD34+ leukemic cells (magenta) show minimal OSMR expression. Nuclei are stained blue. See the article by Reville et al on page 3015.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals









Precision pre-HSCT conditioning by targeting cMPL